Mobile devices, mobile healthcare patient communication apps, and receptive “coaches” can improve the health and well-being of patients with mental or behavioral issues–and even help prevent expensive hospital visits.
 That’s the finding of an innovative pilot program called “coactionHealth” conducted recently by the Nashville-based not-for-profit organization, Centerstone Research Institute (CRI, at right). The coactionHealth team preloaded iPhones with a selection of mobile health apps, and gave the iPhones to over 100 Medicaid patients with mental or behavioral issues such as paranoia and schizophrenia. The team then encouraged patients to regularly use the apps to communicate with their “wellness coaches” for moral or practical support.
That’s the finding of an innovative pilot program called “coactionHealth” conducted recently by the Nashville-based not-for-profit organization, Centerstone Research Institute (CRI, at right). The coactionHealth team preloaded iPhones with a selection of mobile health apps, and gave the iPhones to over 100 Medicaid patients with mental or behavioral issues such as paranoia and schizophrenia. The team then encouraged patients to regularly use the apps to communicate with their “wellness coaches” for moral or practical support.
The pilot program was a resounding success. The mobile apps not only improved timely communication and engagement between the patients and care providers, but also reduced patients’ emergency room visits by 39 percent, and inpatient hospital days by 53 percent.
Patient communication apps critical to success
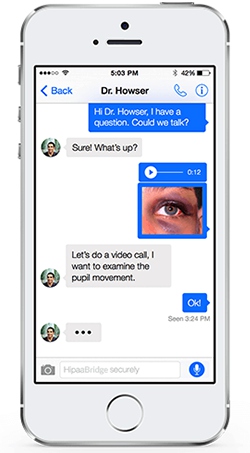 One of the centerpiece patient communication apps was Everbridge’s HipaaBridge, which allowed patients to text and video chat with their coaches–all under a cloak of military-grade security that’s compliant with US HIPAA regulations. This April, the US healthcare accreditation organization called The Joint Commission lifted its ban on texting by clinicians, provided that they use a secure, HIPAA-compliant messaging app.
One of the centerpiece patient communication apps was Everbridge’s HipaaBridge, which allowed patients to text and video chat with their coaches–all under a cloak of military-grade security that’s compliant with US HIPAA regulations. This April, the US healthcare accreditation organization called The Joint Commission lifted its ban on texting by clinicians, provided that they use a secure, HIPAA-compliant messaging app.
In the CRI pilot program, many of the patients used the HipaaBridge app to send their coaches texts and picture messages about their feelings or progress. Some of the other patients preferred to use the app’s video chat feature.
“I could be on my way to visit one patient and while in route, be able to check in with someone who is having a good day–they just wanted to share their progress, says Teresea Higham, a CRI Wellness Coach. “It was very helpful for them to have this outlet. They know they have someone who is listening to them.”
Although Centerstone encouraged such communications, some patients were at first too overzealous with texting or calling, so the program team had to set boundaries as to when patients could contact their coaches, depending on the level of their need.
Overall though, CRI sees patient communication apps and other mobile tools as important, money-saving alternatives to costly, avoidable emergency room visits and hospital stays.
“When it comes to those suffering through extreme mental challenges, many times our patients just wanted to check in with their team of wellness coaches,” says Christina VanRegenmortar, CRI’s Director of the Center for Clinical Excellence and National Policy. “That communication provides an amazing level of comfort for patients.”
“Being able to pick up a smartphone, press a button and securely speak face-to-face with us was a game-changer,” adds Teresea Higham. “Being able to say, ‘I’m checking in. I took my medicine today.’ Or, ‘I’m not feeling well today, the voices are really loud today,’ and then having us be able to immediately talk them through what’s best for them is immensely valuable.”
To learn more about the secure communications behind HipaaBridge and related Everbridge apps, you can check out the company’s profile page here on MobileVillage.





